
Order Safer Sex Supplies Through SHARE
Online orders for safer sex supplies through SHARE Package is open! Orders will be sent to on campus and off campus addresses in the US within 2 weeks.

Order Safer Sex Supplies Through SHARE
Online orders for safer sex supplies through SHARE Package is open! Orders will be sent to on campus and off campus addresses in the US within 2 weeks.
Online abuse is an umbrella term that encompasses many types of behaviors and interactions that are intended to provoke fear, threaten, intimidate, or otherwise harm their targeted person or group. There’s a wide variety of online abuse and harassment, and has impacts outside of the online world from emotional and personal impacts to employment. Regardless, harassment is wrong and depending on how the harassers got information, could be illegal. It is never the victim’s fault.
This may look like sending hateful messages, hacking others’ accounts, stalking, sending threats, non-consensual sharing of intimate or private images, initiating and/or participating in campaigns to spread damaging and/or false information. Here’s a guide if you want more information.
Who is more likely to be on the receiving end of online harassment? Data tells us that often age and gender are closely associated with those who experience harassment, but there are other factors such as sexuality and race.
Some statistics about age and gender (source):
Because there are different ways people are harassed or abused online, here’s a helpful list of terms to use. This is also helpful for when you encounter abuse as a bystander or victim, to better describe what is happening.
Now, the rest of this page is split up into four parts: what to do if you see someone being harassed, what to do when you face harassment, how to keep yourself safe on the internet and online in general, and what you can do as a Reedie.
2. Remember the list of terms? Here’s where that may be helpful!
3. Bystander intervention, The Five D’s: Distract, Delegate, Document, Delay, and Direct. (SHARE has a whole other blog post just about bystander intervention too!) You don’t have to interact directly; there are four other ways to intervene:
II. Distract: You can push back by:
III. Delegate: This supportive community can help you:
IV. Document: Keep in mind, looking at screenshots of abuse can be retraumatizing for those on the receiving end, so when you share the information you’ve collected, be sure to offer a clear trigger warning. You can try something like: “Hey, documenting abuse is really important, but I realize it can also be traumatic, so I’ve taken screenshots and saved hyperlinks for you in this folder. You can just store it somewhere safe in case you need it later.”
V. Delay: You can:
There’s a wide range of ways you might be harassed online. This section is if the harassment you face is stalking, bullying, sharing intimate or private images without permission, or spreading misinformation about you. This is still pretty broad, so there’s a section for each of these along with general information about taking care of yourself after facing harassment.
Stalking/Doxxing
Bullying/Spreading Misinformation
2. As mentioned before, documenting is a good idea for potential future evidence or reporting, along with possibly finding out where the information is coming from and where else it may be going.
3. You can also report the harasser to the social media platforms and ask friends/family/followers to do the same.
Sharing Intimate or Private Images
There are different options going forward, whether to report to law enforcement or the social media platform, conduct an assessment about who’s making the comments or threats, or just securing your profiles.
We know that reaching out to law enforcement is not a viable option for everyone. “The benefit of reporting a threat to law enforcement is that it starts a trail of evidence for your case, in case further threats are made and you decide to take further action in the future.” (OnlineSOS) You can report with a trusted friend or family member if you do not want to go alone. If you do not immediately report, you can always hold onto the evidence and documentation if you decide to report in the future.
These methods to respond are not exclusive to one type of harassment and can be used however you feel safest and is what you want to do.
There are also basic steps you can do to keep yourself safe from harassment and to be more safe on the internet in general
Why do we say “safer” sex?
No matter what type of sex you are having, with who, and with what means of protection, there will always be a degree of risk. We can’t protect ourselves against everything, but we can always be more prepared and take steps to protect ourselves and others. This includes having conversations before having sex about what everyone wants and expects, talking about limits and boundaries, disclosing STD/STI status, and having sexual health supplies like condoms and lube. You can get many of these sexual health supplies from SHARE’s Package form. We also have zines and handouts about emotionally safer sex. This page will provide brief information about that last one – safer sexual health supplies – in this blog post. Read more to learn about the types of protection SHARE offers, information all about lube, and STD/STI’s.
Why use protection? How does it make sex more pleasurable?
Sex can create a lot of emotions because of the chemicals at play in the brain and body, the vulnerability, societal standards, and many other reasons. Specifically there can be a fear of STD/STIs or pregnancy that could prevent someone from having a pleasurable time. Using protection can ease someone’s worry and concerns, making sex more enjoyable because they feel safer.
According to Planned Parenthood, there are 18 types of birth control (which means to prevent pregnancy, and not all of them can be used to prevent STD/STIs). Yes, eighteen! Ranging from the pull out method to sterilization (a vasectomy or getting tubes tied). Some are hormonal and some are a physical barrier. There’s a lot of variety and options for what works best for you.
Here’s Planned Parenthood’s list with pros and cons, and effectiveness. Bedsider also has a comparison tool to help choose between different options.
If you want something easy and free, SHARE supplies external condoms, internal condoms, and oral dams through our order form and when we table! Here’s a little bit more about them:
Condoms and Dental Dams
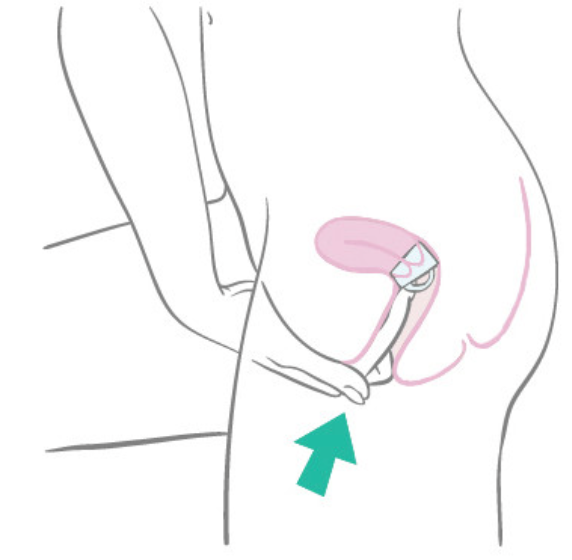
A condom is a physical barrier to prevent pregnancy and to prevent STD/STIs. There are two types: external and internal. An external condom fits snugly around the penis so the semen is inside the condom rather than the vagina. Internal condoms, also called female condoms, are placed inside the vagina rather than over the penis. The FDA approved female condom, called FC2, has a FAQ page for any of your questions.
Condoms can be made of latex, nitrile, polyurethane, polyisoprene, and lambskin (which do not prevent STD/STIs). SHARE supplies latex and latex-free (polyurethane) condoms. When using condoms, remember that they can only be used once, you have to use condoms every time you have sex for them to be effective, and condoms can expire (so check expiration dates). People with sensitivities may also find them irritating. Condoms also come in different sizes, with different types of lube. They also have flavors, colors, and glow in the dark types, too. They are easy to find, and with SHARE’s order form, have no cost!
SHARE also provides dental dams through the order form. Here’s some information about them:
Dental dams are a physical latex or polyurethane barrier for oral sex because you can transmit or receive STD/STI’s from oral sex. They are placed between the mouth and the partner’s genitals or anus. They can also be helpful for if you’re squeamish about oral sex. They stop fluid exchanges, but are not effective for pubic lice, HPV, and herpes.
Like condoms, they can only be used once, have different sizes, colors, and can be flavored or unflavored. You can also make a DIY dental dam out of external condoms if you don’t have any on hand.
Here and here provide more information about dental dams.
Here are some other options that SHARE doesn’t supply, but you might want to consider:
The HCC can also provide prescriptions for hormonal and long term birth control options along with referrals and genital exams.
The next post will be all about lube, toys, and have more resources!
HRT is a medical process in which you take certain medications to create a hormone that your body does not naturally produce. For transwomen or trans femme people, these medications can include spironolactone/aldactone and estrogen/estradiol.
Aldactone is a hormone blocker. This blocks the hormones that produce male secondary sex characteristics. This is typically taken before starting estrogen in order to prevent the effects of testosterone from continuing. People who plan on using both this and estrogen typically start with aldactone 4 to 8 weeks before starting estrogen. In substitute of aldactone, some people may opt for Gn-RH analogs.
Estrogen is the hormone that produces female secondary sex characteristics. It comes in multiple forms: a pill, patch, cream, gel, spray, and shot. These have their own risks and benefits, but they lead to the same outcomes.
Different Forms of Estrogen
Pill form is not recommended for people with a family history of blood clots. However, it is more convenient and less intimidating than injections for many people.
Injections have actually been found to create higher levels of estrogen than pill form. This could make female characteristics present faster or be more noticeable.
Transdermal options (patch, cream, gel, spray) increase estrogen production the least out of these options, but they can work for people who do not want to use needles and have a history with blood clots. They may be inconvenient in that you have to make sure nothing touches where you have applied the medication until it completely dries.
What are the risks and effects of estrogen?
Because of the decrease in testosterone levels, one should expect to experience less interest in sex and fewer erections within the first 3 months of treatment. Also in the first 3 months, one tends to notice less hair loss. From the 3-6 month period is when more full-body changes start to begin. Muscle mass will decrease in exchange for an increase in body fat. Breasts will also begin to develop. The full effect of these changes will be experienced 3-5 years into treatment. Also around the 3-6 month period, testicular atrophy will occur, which is when the balls become smaller. In this same period, people found that their skin became smoother, less oily, and their overall sweat decreased. After this, in the 6-12 month period, one should expect to notice less hair growth on the face and body.
Emotional changes may occur in the beginning of treatment, such as mood swings and increased sensitivity. There can also be shifts in one’s sexuality. These tend to stabilize as treatment continues. Research finds HRT to overall heavily improve one’s mental health.
Some of the effects of HRT can be reversed if one were to stop taking their medication. Traits that tend to be reversed are skin changes and the fat and muscle mass changes. Some effects cannot be reversed, such as breast development and decrease in fertility. If one wishes to slow the effects of HRT, they can take smaller doses of their medication. Tell this concern to your doctor.
There are many risks associated with HRT, such as stroke, blood clots, and high blood pressure. These risks can be prevented if blood tests are regularly conducted to keep one’s estrogen range in the same range as that of a cisgender woman. The chances of one developing breast cancer also increases, as it does when comparing cis women to cis men. Regular breast cancer examinations are encouraged as they are for cis women. There is also potential for a decrease in fertility, or complete loss in it, but this has been less looked into. It is important to note that a lot of studies regarding the use of supplemental hormones occur on patients that already naturally produce that hormone rather than on gender diverse individuals.
Getting started with HRT
Speak with your Primary Care Provider about interest in starting HRT. They may then conduct a physical examination and review your medical history before referring you to a gynecologist or another doctor with experience in hormones (or maybe themself if they prescribe HRT!) The next doctor will likely have you get your blood drawn in order to test your starting levels and moderate them throughout treatment. They will then write your prescription if your levels are not concerning.
Reed is a convenient place to start HRT, with options dependent on insurance. All students at Reed will have some type of insurance coverage. If you are on the school-provided insurance, you are insured by PacificSource. They have a full Gender Affirming Care Team to help you explore your options. Our medical team at Reed can talk with you to discover what parts of HRT may be right for you. To learn what may be covered versus what is not, it is best to reach out to your insurance plan. Once connected, the Health and Counseling Center (HCC) on campus can prescribe your medication for HRT. You can call or walk to their building near 28 West to schedule an appointment. The HCC can also connect you with additional services to support your gender transition, like affirmative therapists, surgery consultations, and more!
Different forms of testosterone
First, there is the most popular: injection. This is used through a small needle injected once a week. Injections are typically in the thighs, stomach, and/or upper-arm depending on type. Injections are often self-administered. Prescriptions for injectable testosterone include the testosterone itself, the syringe, the needle(s), the alcohol wipes, and thorough instructions. Needle disposal waste buckets are also available for free at the HCC and in multiple restrooms across campus. The substance testosterone is put in for injection may cause allergic reactions. This may present as excessive itchiness or redness in the injection site. There are other substances that can be substituted for this, if you report an allergic reaction to your doctor there are other options than completely stopping testosterone.
There is also the transdermal, which is any method that transfers testosterone through skin. This includes patch, but also gel. Gel testosterone must dry on your placement before it touches anything else, or it may come off and influence whatever it touches instead. It is typically applied to parts of the upper body such as arms or stomach, but may also be applied to the front of the thighs depending on which gel type it is.
Then there is a less common pill form of testosterone. Oral testosterone is a newer development and not typically recommended due to risks regarding blood clots andpotential for strokes. It is instead primarily used for AMAB people treating testosterone deficiency.
What are the risks and effects of testosterone?
Many risks associated with testosterone are in regards to AMAB people seeking to increase their naturally occurring levels of testosterone. These risks are not as severe for AFAB people seeking to masculinize their appearance and under the supervision of a medical professional.
It is not advised to take testosterone while pregnant or if you plan to become pregnant. If you are taking testosterone then discover you are pregnant, it is recommended you pause your HRT immediately until you can speak to your doctor. Similarly, if your sexual partner is pregnant, it may be advised you stop taking testosterone depending on which form of it you use (gel/patches). Risks associated with testosterone include blood clotting, liver problems, heart problems, and strokes. Again, these are primarily found in AMAB people than they are with AFAB people who regularly have blood tests and are treated under the care of a qualified doctor.
As for the intended benefits of testosterone, there are quite a few. Many changes are made to the face, including in overall masculinization in face shape, oilier skin, acne, facial hair, thinning of the hair, and development of an Adam’s apple. Acne tends to improve after a year on testosterone and can also be treated with prescribed creams such as benzoyl peroxide by the same doctor who prescribes you the HRT. Thinning of the hair differs in intensity depending on male-patterned baldness in your own family. Receding hairline can also occur.
Body changes are also made. Fat redistributions from hips and thighs to the stomach. Muscle mass increases in the arms and legs. These changes take the longest to fully develop at between 2-5 years. Veins become more prominent. T (short for testosterone) can cause body hair basically anywhere on the body, including but not limited to: the chest, stomach, back, shoulders, arms, legs, butt, pelvis, feet, hands (literally everywhere). The extent of this will be fully realized between 3 and 5 years of T use. People have also noticed changes in bodily scents such as urine, vaginal discharge, or sweat. There is an increase in sweat production.
The voice deepens, which cannot be reversed if one were to stop taking testosterone, however microdosing T can help your voice lower at a more manageable rate, decreasing voice cracks or strain. There is also a myth that T lowering your voice is physically painful to experience, which is not true among most patients.
Taking T can reduce your fertility, though it is important to know that this does not make you infertile. You can still get pregnant and should wear protection/use birth control when in situations where pregnancy may occur if you do not wish to become pregnant. Though you are still fertile, T typically stops or at least reduces menstrual periods. This usually happens within the first few months of taking T.
Emotional changes occur, many people report feeling less emotions less intensely. Some have difficulty crying while on T. T can also change sexual preferences and typically increases libido and overall arousal.
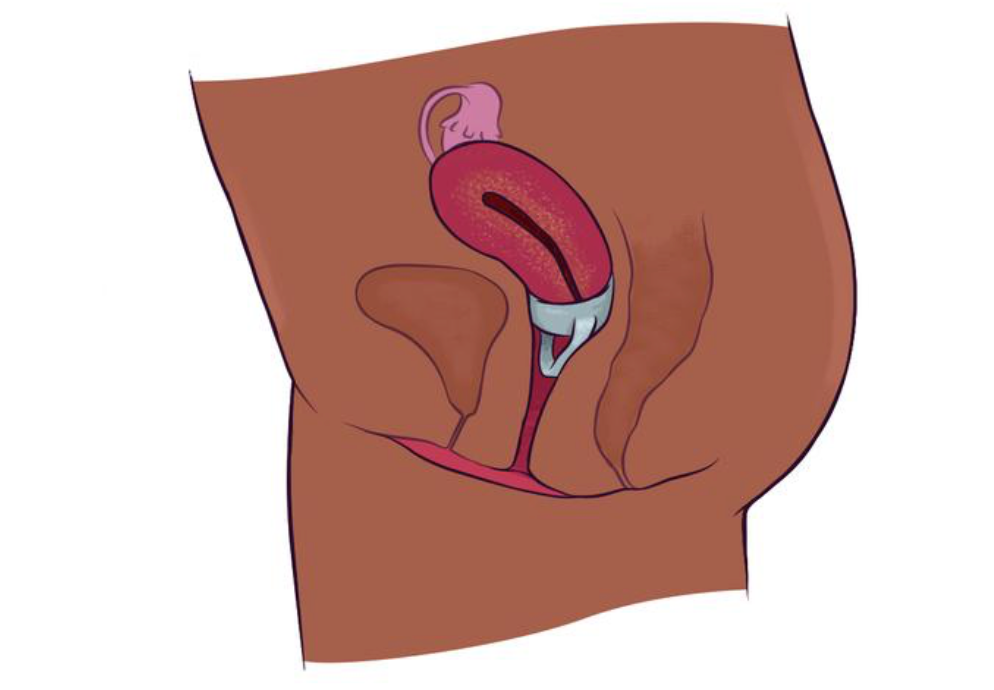
T makes several changes to the vagina: An enlarged clitoris often called ‘bottom growth’ or ‘t-dick’. This is when the clitoris functions as a sort of smaller penis that can become erect and protrude from the clitoral hood. It also can cause vaginal atrophy, which can make it more difficult for the vagina to self lubricate or become wet during sexual intimacy. This can lead to difficulty with penetration that can be helped through pelvic floor exercises, lube, a breathing exercises. Sensations of an orgasm can also change. People say it becomes more centralized to the vagina rather than throughout the whole body.
Getting started with HRT
Speak with your Primary Care Provider about interest in starting HRT. They may then conduct a physical examination and review your medical history before referring you to a gynecologist or another doctor with experience in hormones (or maybe themself if they prescribe HRT!) The next doctor will likely have you get your blood drawn in order to test your starting levels and moderate them throughout treatment. They will then write your prescription if your levels are not concerning.
Reed is a convenient place to start HRT, with options dependent on insurance. All students at Reed will have some type of insurance coverage. If you are on the school-provided insurance, you are insured by PacificSource. They have a full Gender Affirming Care Team to help you explore your options. Our medical team at Reed can talk with you to discover what parts of HRT may be right for you. To learn what may be covered versus what is not, it is best to reach out to your insurance plan. Once connected, the Health and Counseling Center (HCC) on campus can prescribe your medication for HRT. You can call or walk to their building near 28 West to schedule an appointment. The HCC can also connect you with additional services to support your gender transition, like affirmative therapists, surgery consultations, and more!
Oregon’s Medical Protections for Trans Individuals
Since 2014/2015, HRT and gender-affirming surgeries have been approved for insurance coverage. In order to get coverage, one must show a history of struggling with gender dysphoria based on an evaluation from a mental health professional. They must also be able to consent to treatment. For gender-affirming surgeries, one must have the requirements above along with two letters of recommendation from mental health professionals along with 12 months of being on hormone treatment and living as their actual gender.
Gender reassignment surgery is no longer a requirement for a gender change. You can now petition for a gender and name change without having to have specific surgeries or treatment. It is illegal for Oregon health insurance companies (such as PacificSource) to discriminate against customers based gender. They must cover medically necessary treatments if the criteria is met.
Anti-discrimination laws do include trans people, this applies to housing, employment, and public accommodation laws.
America’s Protections for Trans Individuals
Name changes and gender change laws vary by state in terms of whether or not it is legal and what criteria must be met in order to do so. Therefore, being trans is not a protected class in America, meaning anti-discrimination laws do not inherently apply to trans people. Trump has stated that he plans on discouraging each state from allowing gender-affirming care to people of any age, including adults. This has yet to actually be implemented and ultimately this area of care relies on the individual state.
Surgical Options
For binary trans people, it is typically recommended that you start HRT before getting surgery so that your body’s fat and muscle redistribution aids the surgeon in finding your body’s natural contour. However, this isn’t a requirements for surgery and can be pretty irrelevant to nonbinary trans people seeking surgery.
There are many options for people seeking feminizing surgery. For instance, there is facial feminization surgery which has the goal of achieving softer facial features through the use of jaw contouring, shaving down the brow bone, rhinoplasty (nose surgery), and/or shaving down the adam’s apple.
There is also breast augmentation or top surgery. Breasts naturally develop from HRT, but if one wishes to make the breasts appear fuller they may opt for breast augmentation which is when breast implants are inserted into the chest area.
Then there is body contouring, which primarily uses liposuction to create a feminine hourglass shape to the body. HRT can help in changing body shape, but this is for people who seek to see a larger difference in effect.
Vaginoplasty/bottom surgery is also an option. It uses the already present tissue to create a more vaginal like appearance and aesthetic. This is the most common surgery when it comes to altering the genitals, but there are other options. These include removing the testicles (orchiectomy), removing the penis (penectomy), or creating a vulva but not a vagina (vulvoplasty).
Voice surgery can also be done to adjust the vocal cords to make a higher-pitched voice. Voice training is also often used by MTF individuals to practice using a more feminine voice, as HRT does not impact voice.
Transmasculine individuals have similar surgical options. Most common is a mastectomy or top surgery, which is a procedure in which breast tissue is removed from one’s chest. It is important to note not ALL breast tissue is removed, which means one still has a chance of developing breast cancer even after this surgery. There are different types of mastectomies depending on one’s body shape and desired aesthetic. Nipples can also be removed (or kept) through top surgery.
Then there is facial masculinization surgery which is used to create a more masculine face shape by generally having sharper angles or features by contouring the jaw and cheeks, creating a wider forehead, and increasing the prominence of an adam’s apple. HRT does already masculinize the face, but this is to further increase the masculinity of the face.
A common surgery in general is a hysterectomy. This removes the uterus from the body. There are different types of hysterectomies that can remove different amounts of female organs in the body, but all include the uterus. This makes it so the body no longer naturally produces estrogen, you can no longer get pregnant, and you will no longer menstruate.
Lastly, there is phalloplasty/bottom surgery. It is usually used with a scrotoplasty (creating testicles) to create a penis. Outside of aesthetics, functionality differs when it comes to sex and depends on the type of bottom surgery one gets. Advanced bottom surgery can include a pump of sorts in order to become erect while others don’t. Instead of phalloplasty/scrotoplasty, one can also opt for less common surgeries such as metoidioplasty or vaginectomy. A metoidioplasty creates a penis from the clitoris, this does require you to be on HRT to enlarge the clitoris beforehand. A scrotoplasty is typically used with this surgery as well. A vaginectomy is when the vagina is removed, it is for people who do not plan on a form of bottom surgery that constructs a penis.
HRT for Feminizing AMAB Bodies
Trans and Gender Nonconforming Students – Health & Counseling
Services – Reed College
Estradiol levels higher with injection vs oral, transdermal HT for
transgender women
Feminizing hormone therapy – Mayo Clinic
MTF Hormone Therapy: A Guide to Physical and Emotional Change
Can Transgender Hormone Transition Therapy Be Reversed? – Healor
MTF Before and After – Gender Confirmation
Transgender Health Program: Hormone Therapy | OHSU
HRT for Masculinizing AFAB Bodies
Testosterone (topical application route) – Mayo Clinic
Female-to-male testosterone: What to know
HRT Timeline and Effects: Hormone Replacement Therapy Info
Bottom Growth 101: Everything You Need to Know Before Starting
Testosterone | Them
Legal Rights and Surgeries
Federal Civil Rights Law Doesn’t Protect Transgender Workers, Justice
Department Says
Male-to-Female Transgender Surgery
Gender Affirmation Surgery: What Happens, Benefits & Recovery
Transgender Hysterectomy Guide
Other Resources
Trans Portland | Linktree mental health, trans resources, and community in
the Portland area
Post-Election 2024 Anti-Trans Risk Assessment Map
Groups at Q — Q Center support & affinity groups for LGBTQ+ persons
Gender Affirming Care Team PacificSource
○ GenderAffirmationTeam@PacificSource.com | 888-977-9299; for students on Student Health Insurance to find care locally and connect to resources
LGBTQ Care | Planned Parenthood Columbia Willamette
World Professional Association of Transgender Health
Trevor Lifeline crisis intervention and suicide prevention services to
lesbian, gay, bisexual, transgender, queer and questioning (LGBTQ+)
young people
Q Center Portland facilitates weekly and monthly discussion and support
groups for transgender and gender non-conforming people
Outside In provides transgender and gender diverse healthcare in
Portland
OHSU Transgender Health Program provides gender affirming healthcare, as well as support and advocacy services
Transgender Resources compiled by GLAAD
Be an Ally – Support Trans Equality, composed by the Human Rights
Campaign
Guide to being an ally to transgender and non-binary young people by the
Trevor Project
The Movement Advancement Project provides state-by-state analyses of
LGBTQ+ policy, including transgender healthcare.
Basic Rights Oregon has broadly compiled a list of rights and resources
for LGBTQ2SIA+ Oregonians.
Local resources for sexual health care & victims assistance are listed on
the SHARE webpage for sexual health and survivors resources. Our
providers in the HCC can help connect you to medical care on and o
campus.

Confidential Advocacy & support is available to all Reed students!
Contact L. Mattson directly at mattsonl@reed.edu or via our Advocacy Contact Form. Response within 48-72 hours.